A study from Department of Surgery, University of Washington, Seattle, Washington
Background/Objective: Intraoperative Digital Specimen Mammography (IDSM) has become the standard confirmation method to ensure an image guided procedure has removed the targeted breast lesion. We've seen improvements in camera acuity, faster processing and larger fields of view to facilitate the surgeon's identification of non-palpable cancers. The guidelines for clear margins have also been changing during this time. To obtain the so-called three-dimensional view (3-D), routine use of two orthogonal images have been utilized as a 3-D view. Yet in screening mammography, true 3-D mammography has now arrived as tomosynthesis, not simply two orthogonal MLO and CC views of the breast. Likewise for specimen imaging, true 3-D mammography is specimen tomosynthesis, not two orthogonal views using a 2-D machine. We report our current findings on the enhancement of specimen imaging provided by true 3-D intraoperative specimen tomosynthesis (IDST).
Methods: Between April 2015 and October 2016 we have obtained specimen imaging on 210 consecutive image-guided breast lumpectomies using two specimen imaging machines. One provided IDSM and the other provided IDST. Two orthogonal views of each specimen were taken with each machine. For patient management, intraoperative review of all images was available to the operating surgeon for their immediate action as appropriate. Comparison data was accumulated as to ease of use, time to first image, handling issues, re-excisions, mechanical issues as well as image comparisons. Images of breast lesions were categorized into three groups by their dominant findings: 1) densities, 2) calcifications and 3) clips. All images were forwarded from the operating room to the radiologists and permanent recording via standard PACS system.
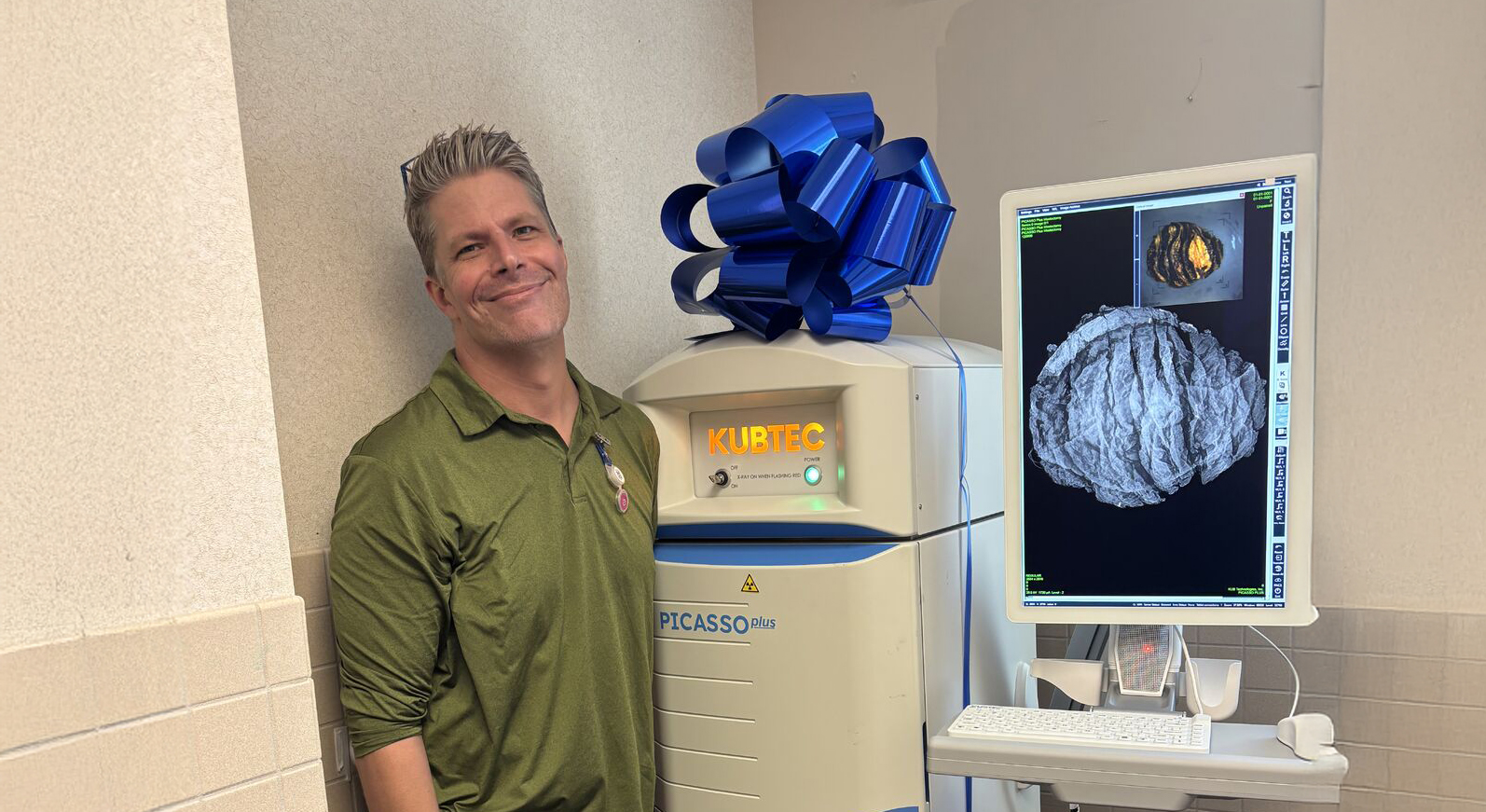
Results: The circulating nurse received the specimen from the surgeon and placed it sequentially in each of the machines in the exact same orientation. For equal comparisons, two orthogonal views were taken with each device, although the use of tomosynthesis obviates the need for two orthogonal images since the Z-axis is visible on a single image. Functionality of the two machines were very similar. Time to first image was prompt although there was a difference in the developing time for the IDST, being almost twice as long as IDSM (65 seconds vs. 32 seconds). Of the 210 patients, specimen images were classified into 61% densities, 26% clips and 13% calcifications. The primary difference in imaging was found in the density group. In 70% of patients with densities or spiculated lesions, the IDST provided more information than the IDSM. It was possible to see the target lesion more often with IDST than IDSM. Comparing the same image orientation, overlapping tissue was avoided and spiculations could be seen more easily using IDST (see figure). Looking at all 210 lesions as a group, IDST was more precise in 43% of all lesions examined. This was reflected over the time of the study as surgeons would only look at the IDST to assess their intraoperative excision accuracy and need for immediate re-excision.
Conclusions: Use of specimen tomosynthesis in the operating room has improved the accuracy of intraoperative imaging in 43% of cases. By improved visualization of the cancer, the surgeon can be sure they have removed the target lesion and not only the clip. Further use by others should validate these early findings.
Request your personal meeting or demo
Fill out the form and one of our exhibition managers with be in touch about scheduling your personal meeting or demo at our upcoming trade show.
For more news, views, & events, please visit our LinkedIn page
Click Here