In the fast-paced environment of a gross room, accuracy and efficiency are paramount. Every tissue sample processed plays a crucial role in patient care, so proper and timely specimen evaluation from the outset can significantly impact diagnostic accuracy and treatment decisions. This is where specimen radiography steps in, providing real-time imaging to support Pathologists' Assistants (PAs), Pathology Residents, and Pathologists in their daily workflow.
What Are Pathologists’ Assistants Trying to Achieve?
Pathologists’ Assistants (PAs) are essential in the gross room, performing a range of tasks to ensure high-quality patient care. The main role involves assessing and describing the gross features of surgical specimens, carefully sectioning them for microscopic evaluation, and generating a dictated gross report that aligns with the findings1.
- Confirming specimen orientation and key anatomical landmarks to ensure precise sectioning.
- Identifying and grossly assessing margins to determine excision completeness and guide treatment decisions.
- Detecting critical markers such as surgical clips and microcalcifications that impact diagnosis.
- Maintaining workflow efficiency by minimizing delays and ensuring rapid case turnaround.
With the high-volume demands of surgical pathology, maintaining both efficiency and accuracy is essential.
Grossing Challenges Without Specimen Radiography
Without specimen radiography, grossing is a more complex, time-consuming process, with additional steps, and increased chance for error. Key structures like microcalcifications or clips are often invisible or hard to see by the naked eye, sometimes causing substantial time to be spent trying to find them and also increasing the risk of submitting non-diagnostic or non-informative sections, leading to re-grossing and further lost time.
In the case of a clip, it must be retrieved to ensure that the exact prior biopsy site has been sampled for histological evaluation. When the clip can’t be found grossly, a radiograph is very often the only solution.
Why Not Use Existing Radiology X-ray Systems?
Some PAs that see the value of specimen radiography will resort to sending their specimens over to the radiology department for imaging. However, this can result in radiology workflow interruptions, as well as delays to pathology examination and overall turnaround time.
“When a radiograph is required, a pathologists’ assistant, pathology resident or fellow makes an appointment (typically for the same day or next day), hand-carries the specimen to the mammography suite (7 min’ walk from pathology), and obtains the necessary image with the assistance of a radiology technician and radiologist”4.
Transporting specimens to radiology or mammography is a time-consuming process that often pulls the PA away from the grossing bench, affecting overall turnaround time and potentially delaying other patient results. Additionally, it could put breast specimens at risk of falling outside the CAP-recommended formalin fixation window of 6 to 72 hours. Furthermore, PAs must rely on radiology staff, leading to potential miscommunication and delays, caused by inconsistent positioning & orientation making it harder to ensure that all critical anatomical structures are adequately visualized.
There is also the potential for suboptimal image quality – Systems in the radiology department are often optimized for imaging entire body parts, not small, excised specimens. This can result in lower resolution and inadequate detail, making it difficult to assess margins or identify key structures like microcalcifications.
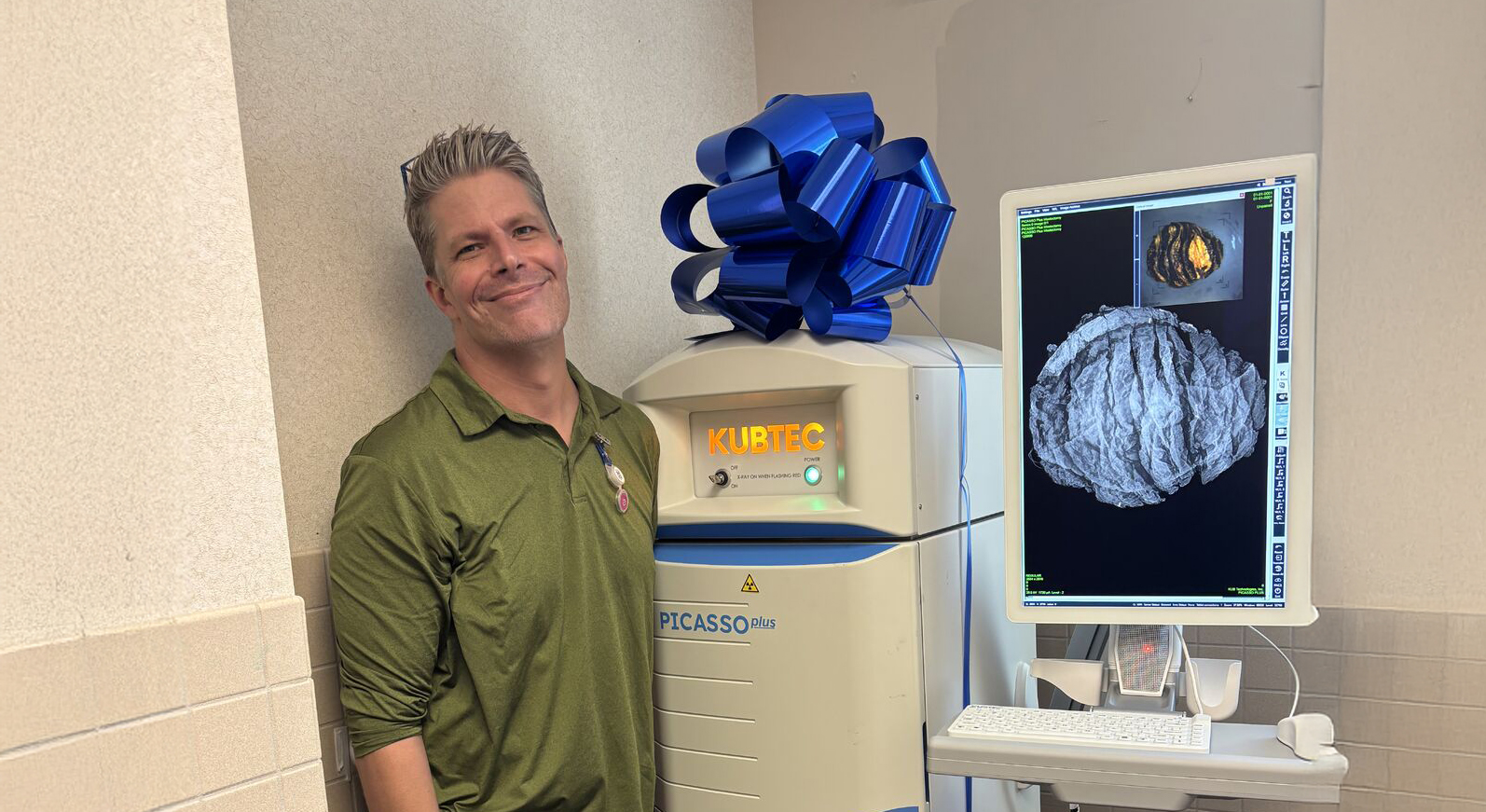
With a dedicated specimen radiography system in the gross room, these problems go away. PAs can capture high-resolution X-ray images in real time, confirming specimen orientation, verifying margins, and ensuring the accurate identification of critical anatomical structures. X-ray imaging is even more impactful when combined with optical imaging, as is the case with Image Blender™— KUBTEC’s exclusive dual-modality imaging technology — which enables PAs to effortlessly overlay X-ray and optical images, making it even easier to pinpoint key structures.
Try the KUBTEC Image Blender™ Here
How Specimen Radiography Enhances Grossing
Breast Specimen Evaluation and Preparation
Breast specimen evaluation is a routine but critical task in the gross room. Without in-gross-room specimen radiography, verifying key features can feel like working blindfolded—as microcalcifications and clips often aren’t visible easily.
- Clip Localization – Confirm surgical clip presence and placement before submitting sections, avoiding delays and additional requests.
- Microcalcification Detection – No more second-guessing. X-ray ensures these tiny but crucial features make it to histology, reducing rework.
- Improved Workflow – No more waiting on radiology. Dedicated specimen imaging accelerates case processing and minimizes disruptions.
Gross rooms using KUBTEC Pathology Specimen Imaging systems report major workflow improvements, cutting breast specimen grossing time from 1–2 hours to just 30–45-minute (Source: Jay Innerhofer, PA (ASCP)cm, Clinical Lecturer-Dept of Pathology – UNM; 20243)
Beyond Breast—Expanding Applications
While in-gross-room radiography is often considered essential for breast specimens, specimen radiography systems from KUBTEC can also help to enhance accuracy and efficiency across a wide range of specimen types.
- Bone & Orthopedic Specimens – Confirms fractures, lesions, and hardware placement for comprehensive evaluation.
- Lung & Thoracic Specimens – Identifies calcifications, nodules, ground glass opacities, and other crucial structures that may be overlooked grossly.
- Head & Neck Specimens – Aids in locating small tumors, surgical clips, or bone involvement for precise sampling.
Conclusion: A Must-Have Tool for the Modern Gross Room
In-gross-room specimen imaging eliminates delays, reduces re-grossing, and ensures precise, efficient specimen evaluation. By offering real-time confirmation of margins, orientation, and critical structures, it enables PAs to work faster and with greater confidence.
With the right tools, the modern gross room becomes a hub of efficiency, precision, and streamlined workflow—enhancing both pathology teams' performance and patient care.
References
- https://thepathologist.com/issues/2020/articles/jun/bridging-the-gap
- https://www.pathassist.org/
- Source: Jay Innerhofer, PA (ASCP)cm, Clinical Lecturer-Dept of Pathology – UNM; 2024
- https://bmcmedimaging.biomedcentral.com/articles/10.1186/s12880-021-00589-1
Request your personal meeting or demo
Fill out the form and one of our exhibition managers with be in touch about scheduling your personal meeting or demo at our upcoming trade show.
For more news, views, & events, please visit our LinkedIn page
Click Here